DROGHE E CERVELLO: FORSE NON TUTTI GLI EFFETTI SONO DANNOSI
20 Ottobre 2017
DECRETO LEGISLATIVO 15 settembre 2017, n. 145
14 Novembre 2017Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study
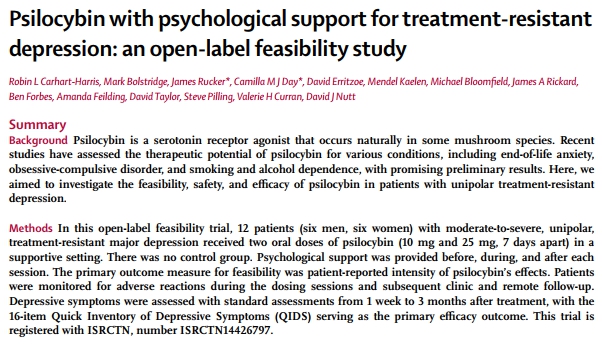
Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study
Robin L Carhart-Harris, Mark Bolstridge, James Rucker*, Camilla M J Day*, David Erritzoe, Mendel Kaelen, Michael Bloomfi eld, James A Rickard, Ben Forbes, Amanda Feilding, David Taylor, Steve Pilling, Valerie H Curran, David J Nutt
Summary
Background Psilocybin is a serotonin receptor agonist that occurs naturally in some mushroom species. Recent studies have assessed the therapeutic potential of psilocybin for various conditions, including end-of-life anxiety, obsessive-compulsive disorder, and smoking and alcohol dependence, with promising preliminary results. Here, we aimed to investigate the feasibility, safety, and effi cacy of psilocybin in patients with unipolar treatment-resistant depression.
Methods In this open-label feasibility trial, 12 patients (six men, six women) with moderate-to-severe, unipolar, treatment-resistant major depression received two oral doses of psilocybin (10 mg and 25 mg, 7 days apart) in a supportive setting. There was no control group. Psychological support was provided before, during, and after each session. The primary outcome measure for feasibility was patient-reported intensity of psilocybin’s eff ects. Patients were monitored for adverse reactions during the dosing sessions and subsequent clinic and remote follow-up. Depressive symptoms were assessed with standard assessments from 1 week to 3 months after treatment, with the 16-item Quick Inventory of Depressive Symptoms (QIDS) serving as the primary effi cacy outcome. This trial is registered with ISRCTN, number ISRCTN14426797.
Findings Psilocybin’s acute psychedelic eff ects typically became detectable 30–60 min after dosing, peaked 2–3 h after dosing, and subsided to negligible levels at least 6 h after dosing. Mean self-rated intensity (on a 0–1 scale) was 0·51 (SD 0·36) for the low-dose session and 0·75 (SD 0·27) for the high-dose session. Psilocybin was well tolerated by all of the patients, and no serious or unexpected adverse events occurred. The adverse reactions we noted were transient anxiety during drug onset (all patients), transient confusion or thought disorder (nine patients), mild and transient nausea (four patients), and transient headache (four patients). Relative to baseline, depressive symptoms were markedly reduced 1 week (mean QIDS diff erence –11·8, 95% CI –9·15 to –14·35, p=0·002, Hedges’ g=3·1) and 3 months (–9·2, 95% CI –5·69 to –12·71, p=0·003, Hedges’ g=2) after high-dose treatment. Marked and sustained improvements in anxiety and anhedonia were also noted.
Interpretation This study provides preliminary support for the safety and effi cacy of psilocybin for treatment-resistant depression and motivates further trials, with more rigorous designs, to better examine the therapeutic potential of this approach.
Funding Medical Research Council.
Copyright © Carhart-Harris et al. Open Access article distributed under the terms of CC BY.
Introduction
Psilocybin is a naturally occurring plant alkaloid found in the Psilocybe genus of mushrooms. Psilocybe mushrooms have been used for millennia for healing purposes, but were only discovered by modern science in the late 1950s.1,2 Psilocybin is a prodrug of psilocin (4-hydroxy-dimethyltryptamine), a serotonin receptor agonist and classic psychedelic drug whose principal psychoactive eff ects are mediated by serotonin 2A (5-HT2A) receptor agonism.3 Psilocybin therefore has a novel pharmacology in the context of currently available antidepressant medications, because selective serotoninreuptake inhibitors are not direct 5-HT2A receptor agonists. Enhanced cognitive fl exibility,4 associative learning,5 cortical neural plasticity,6 and antidepressant responses have been reported with 5-HT2A receptor agonism in animals,7 and increased and sustained improvements in wellbeing8 and optimism9 have been observed after psychedelic experiences in human beings. Findings from human imaging studies with psilocybin have supplemented these discoveries, showing changes in brain activity suggestive of antidepressant potential; for example, a range of eff ective antidepressant treatments have been found to normalise hyperactivity in the medial prefrontal cortex and we found reduced blood fl ow in this region with intravenous psilocybin.10 Moreover, data obtained from large-scale population studies have recently challenged the view that psychedelics negatively aff ect mental health,11–13 with one study’s fi ndings showing lower rates of psychological distress and suicidality among people who had used